Fact check: non-invasive PGT-A
What is PGT-A?
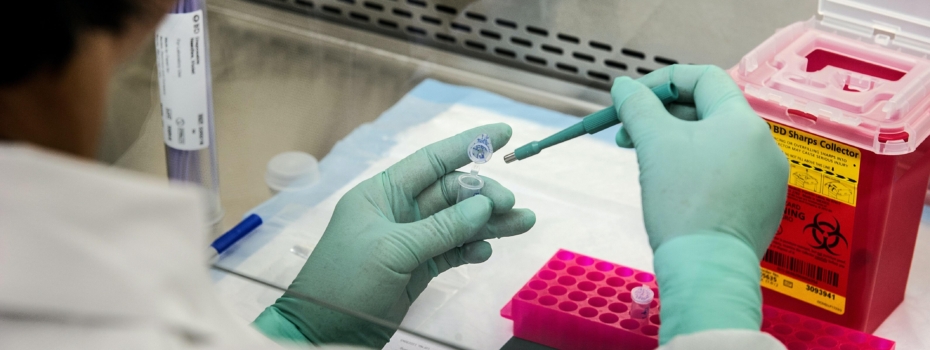
The quest for improving the live birth rate in IVF is never-ending and one important component is embryo selection. This has led to the development of Preimplantation Genetic Testing for Aneuploidy (PGT-A). The traditional method of PGT-A offered at Flinders Fertility and most other clinics involves biopsying the outer part of an embryo (the trophectoderm) at blastocyst stage and then performing an assessment through DNA amplification to identify the number of chromosomes. Embryos with normal chromosome numbers are then selected for transfer.
Are there any risks?
Studies show that PGT-A reduces the time to pregnancy and reduces the risk of miscarriage. However, there are several limitations to the technology such as the risk of potential loss of embryos during the biopsy, and the presence of mosaicism (providing inconclusive results). Studies so far show that PGT-A is not associated with an increase in live birth rates or cumulative pregnancy rates, and in fact, there may be a reduced cumulative pregnancy rate. So the search for the best method to select the genetically normal embryo which is robust and results in a live and healthy birth continues.
What is non-invasive PGT-A?
One such method still undergoing research and currently being offered at some clinics is non-invasive genetic testing of embryos (ni-PGT-A). This method relies on extracting DNA from the culture media in which the embryo has developed. Currently, the accuracy of this method is being tested by comparing it with the results of standard PGT-A (ie trophectoderm biopsy), which in itself is not perfect at this stage as it is limited by mosaicism. The current rate of concordance between non-invasive and conventional PGT-A varies between 50-70%, which means that the results are far less reliable than conventional PGT-A technology. This is insufficient for Flinders Fertility to recommend non-invasive PGT-A at the present time.
Limitations of non-invasive PGT-A
There are other limitations of non-invasive PGT-A. Unlike standard PGT-A, only embryos created using ICSI are suitable for assessment and these are known to have inferior outcomes compared to standard IVF. Currently, ICSI is recommended only if there is a risk of failed fertilisation with standard insemination, or where there is severe male factor infertility.
Other challenges for non-invasive PGT-A include:
- a lower yield of cell-free DNA, making assessment less reliable (hence the higher error margin between the two technologies)
- maternal contamination requiring the removal of all cumulus cells from the oocyte
- the need for extended culture to obtain a sufficient yield of DNA, and its unknown impact on developmentally competent embryos
- a higher chance of failed DNA amplification, and
- the process of release of cell-free DNA into the culture medium, which is still the subject of research
Therefore, several technical challenges need yet to be addressed before accepting non-invasive PGT-A as a reliable source of identifying chromosomally normal (euploid) embryos.
Well-designed studies are required to determine how accurately cell-free DNA represents the genetic constitution of the whole embryo and to evaluate the clinical efficacy of these methods on pregnancy outcomes. Flinders Fertility in conjunction with PerkinElmer is currently involved in one such study.
In summary
Until we have robust evidence for the efficacy and safety of non-invasive PGT-A, standard trophectoderm biopsy for PGT-A remains the optimal method for obtaining embryo-derived DNA for PGT-A.
Want to find out more?
For more information on PGT-A screening click here. If you have any further questions, you can also arrange a nurse chat with one of our fertility nurses.
For health and wellness information on how to increase your chances of conception, check out our Fertility News page, or download our e-book below.

